COPD, short for chronic obstructive pulmonary disease, is a long-term lung condition that makes it hard to breathe. It is a common illness often caused by smoking, and it affects millions of people worldwide. In COPD, the lungs become damaged and inflamed, leading to narrowed airways and less oxygen flow. Over time, it becomes more difficult to exhale fully, which can leave you feeling short of breath.
In this article, we will explain COPD in simple terms, including what it is, what causes it, the common symptoms, how doctors diagnose it, and what treatment options are available. Our goal is to help you understand this condition and how it can be managed to improve quality of life.
What is COPD?
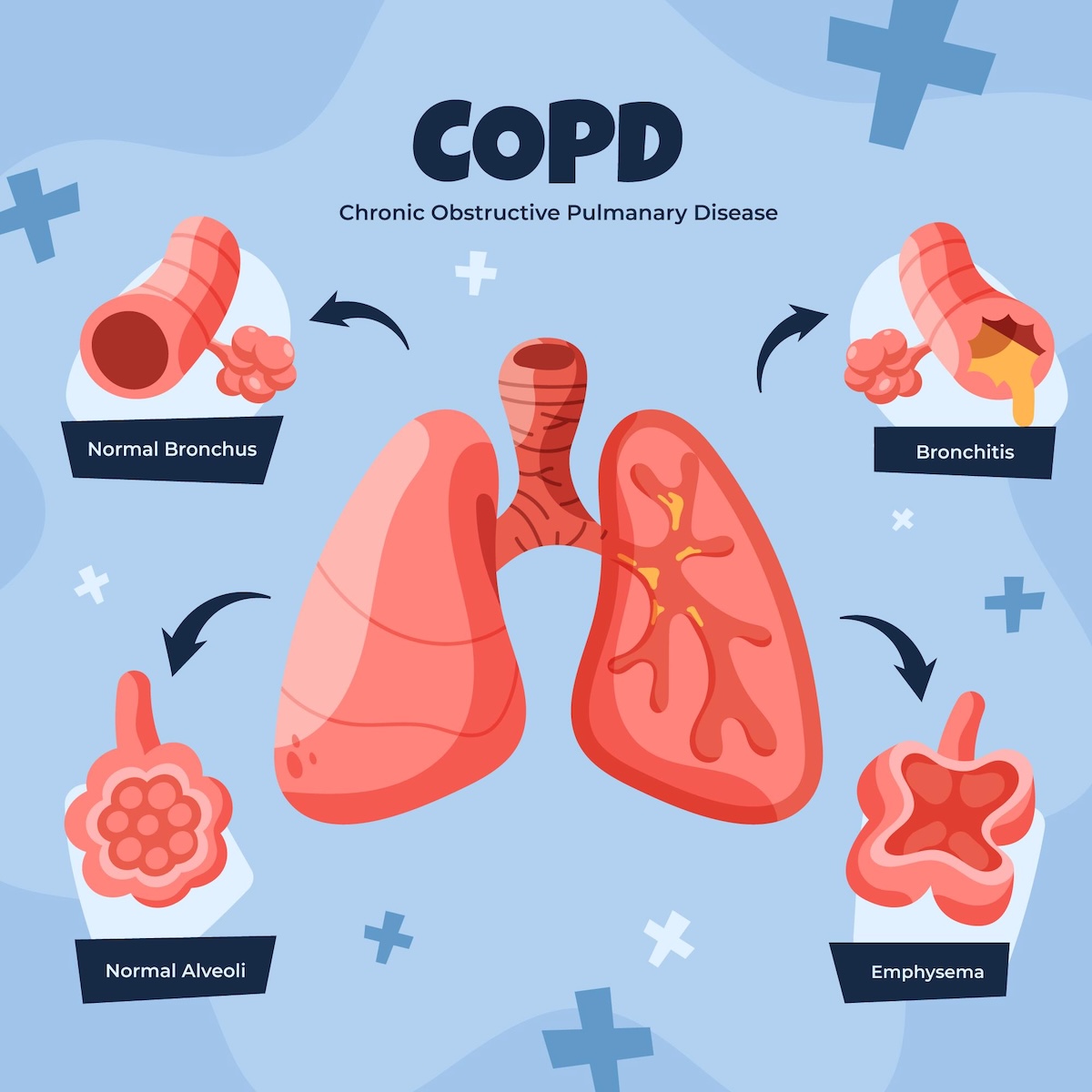
COPD is a chronic (ongoing, long-lasting) lung disease that causes obstructed airflow in the lungs. “Obstructive” means the airflow out of your lungs is partially blocked. People with Chronic Obstructive Pulmonary Disease have trouble moving air in and out of the lungs because the airways are narrowed and the lung air sacs are damaged. This damage is usually irreversible, meaning it cannot be fully healed, but proper treatment can help you breathe easier.
COPD is not just one illness but a term that includes two main conditions:
-
Chronic bronchitis: This is long-term inflammation of the bronchial tubes (airways) accompanied by a cough and excessive mucus production. The swollen airways and extra mucus make it hard to breathe.
-
Emphysema: This is damage to the tiny air sacs in the lungs (called alveoli). In healthy lungs, these sacs are elastic and exchange oxygen and carbon dioxide. In emphysema, the air sacs are destroyed or enlarged, which makes it difficult to get enough oxygen and to push air out of the lungs.
Most people with COPD have a combination of both chronic bronchitis and emphysema to some degree. These conditions cause similar problems with airflow, leading to the typical breathing difficulties of COPD.
Causes and Risk Factors
The primary cause of COPD is long-term exposure to irritants that damage your lungs, especially cigarette smoking. In fact, most people who develop COPD either smoke or used to smoke. Tobacco smoke irritates and inflames the airways, causing scarring and damage over time. However, smoking is not the only cause. Other causes and risk factors include:
-
Secondhand smoke: Regular exposure to other people’s cigarette smoke can contribute to COPD.
-
Air pollution and fumes: Breathing in pollution, chemical fumes, dust, or other irritants (for example, in certain work environments like factories or mines) over many years can damage the lungs.
-
Biomass exposure: In some parts of the world, burning wood, coal, or crop residue for cooking or heating in poorly ventilated spaces can cause COPD after years of inhaling the smoke.
-
Genetics: A rare genetic condition called alpha-1 antitrypsin deficiency can make a person much more susceptible to COPD. People with this condition have low levels of a protein that protects the lungs. If they inherit this deficiency, they can develop COPD even without smoking (often at a younger age).
Certain factors make COPD more likely. These include being over the age of 40 (symptoms usually appear in mid-life or later), having a history of asthma or frequent lung infections, and of course, a history of smoking. Not everyone who smokes will get COPD, but the chances increase with the amount and duration of smoking. The best way to prevent COPD is to avoid smoking and other lung irritants altogether.
Symptoms of COPD
COPD usually develops slowly, so symptoms might not be noticeable at first. Early symptoms are often mild, and people may mistake them for a common cold or simply “getting older.” Over time, as more lung damage occurs, symptoms become more obvious. Common signs and symptoms of COPD include:
-
Shortness of breath (dyspnea): Feeling out of breath, especially during physical activity or when climbing stairs. You might feel like you can’t take a deep breath.
-
Chronic cough: A persistent cough that lasts for months. It’s often a “smoker’s cough” that produces mucus (phlegm). The mucus can be clear, white, yellow, or greenish.
-
Wheezing: A whistling or squeaky sound when you breathe, caused by narrowed airways.
-
Chest tightness: You may feel as if you have to work harder to breathe, or a tight, heavy feeling in the chest.
-
Excess mucus production: Frequent throat clearing or coughing up sputum, especially first thing in the morning.
-
Fatigue: Feeling tired or lacking energy, since less oxygen is getting around your body.
-
Frequent respiratory infections: People with COPD often get more colds, flu, or lung infections like bronchitis and pneumonia.
-
Blue lips or fingernails (cyanosis): In later stages, low oxygen levels in the blood can cause a bluish tint to the lips or nail beds.
-
Unintended weight loss: In advanced COPD, some people lose weight because breathing takes a lot of energy.
-
Swollen ankles or feet: This can happen in advanced COPD due to strain on the heart (a condition called cor pulmonale).
These symptoms usually worsen over time if the lung damage continues. Many people with early COPD only notice a mild shortness of breath or a slight chronic cough. As the disease progresses, even daily activities like walking or getting dressed may cause breathlessness. COPD symptoms can also flare up in episodes called exacerbations (flare-ups), where they suddenly get worse than usual for a few days or weeks. Flare-ups can be triggered by infections (like a cold or flu), air pollution, or other irritants. It’s important to seek medical help if you experience a sudden worsening of symptoms, such as extreme difficulty breathing or coughing up more mucus than normal.
How is COPD Diagnosed?
If a healthcare provider suspects Chronic Obstructive Pulmonary Disease based on your symptoms and history (such as a long-term smoking history or exposure to lung irritants), they will perform a few tests to confirm the diagnosis:
-
Medical history and exam: The doctor will ask about your symptoms (for example, how long you’ve had a cough or shortness of breath) and any exposure to risk factors like smoking or occupational dust/chemicals. They will also listen to your lungs with a stethoscope for wheezing or other abnormal sounds.
-
Spirometry (lung function test): This is the most important test for diagnosing COPD. You will be asked to take a deep breath and then blow into a tube attached to a machine (called a spirometer) as hard and fast as you can. The spirometer measures how much air you can exhale and how quickly. People with COPD have reduced airflow when they breathe out. Spirometry can detect COPD even in early stages, and it can also show how severe the condition is.
-
Peak flow and lung volume tests: Sometimes, additional breathing tests are done to measure how much air your lungs can hold and how well gases like oxygen move from your lungs into your blood. These tests further assess lung function.
-
Chest X-ray or CT scan: Imaging tests can help visualize the lungs. A chest X-ray might show signs of COPD, such as lungs that are larger than normal (due to trapped air) or an expanded chest (barrel chest), and it can also rule out other problems like pneumonia or tumors. A CT scan provides a more detailed look and can detect emphysema or other structural changes in the lungs. Imaging can also help rule out lung cancer or other conditions if needed.
-
Blood tests: One example is an arterial blood gas test, which measures the levels of oxygen and carbon dioxide in your blood to see how well your lungs are getting oxygen into your body and removing carbon dioxide. Another blood test can check for the genetic alpha-1 antitrypsin deficiency if COPD is suspected in someone who is younger or has no obvious risk factors.
-
Pulse oximetry: This is a simple test using a sensor clipped to your finger that measures the oxygen saturation in your blood. It helps determine if you might need supplemental oxygen.
-
Electrocardiogram (EKG): In some cases, if there’s uncertainty whether symptoms are from a lung issue or possibly a heart problem, an EKG may be done to check heart function. (Heart conditions can also cause shortness of breath, so doctors sometimes want to rule those out.)
Often, COPD is underdiagnosed because people may not seek medical care for early symptoms. If you have risk factors (like a significant smoking history) and notice breathing issues, it’s important to see a doctor for evaluation. Early diagnosis allows for earlier management, which can improve your quality of life and slow the progression of the disease.
Treatment Options for COPD
There is currently no cure for COPD, but there are many treatments that can help control symptoms, improve breathing, and enhance your quality of life. A comprehensive treatment plan usually includes lifestyle changes along with medications and other therapies. The specific treatments recommended will depend on how severe your COPD is. Here are the common approaches:
-
Quit smoking: The most crucial step for anyone with COPD who smokes is to stop smoking. Quitting smoking can slow down the progression of COPD and prevent further lung damage. It’s never too late to quit. Doctors can provide resources like counseling, nicotine replacement (patches, gum, lozenges), or medications to help you quit, and support programs to increase your chances of success. Also, avoid secondhand smoke and other irritants as much as possible.
-
Medications (inhalers and more): Many COPD medications are taken using inhalers or nebulizers (devices that turn liquid medicine into a mist you can inhale). The main types include:
-
Bronchodilators: These medicines relax the muscles around the airways, helping to open them up. This makes it easier to breathe and can relieve shortness of breath and wheezing. Bronchodilators come in short-acting forms (for quick relief when you are having trouble breathing) and long-acting forms (used daily to keep airways open). They are often delivered via a handheld inhaler or a nebulizer machine. Examples include albuterol (a quick-acting inhaler) and tiotropium (a long-acting inhaler).
-
Inhaled corticosteroids: These are anti-inflammatory medications that you breathe in. They reduce inflammation in the airways and can help prevent flare-ups. Steroid inhalers are especially useful if you have frequent exacerbations of COPD. (Examples of inhaled steroids include fluticasone and budesonide.) Some inhalers combine a steroid with a bronchodilator in one device for convenience.
-
Other medications: In some cases, doctors might prescribe additional medicines. For example, a drug called roflumilast (a phosphodiesterase-4 inhibitor) may be used for severe COPD with chronic bronchitis to reduce inflammation and prevent exacerbations. Another medicine, theophylline, is an older oral drug that can help with breathing in some cases, though it’s used less often now due to possible side effects and the need for monitoring.
-
Antibiotics: While not a routine daily treatment, antibiotics are often used when someone with COPD gets a bacterial lung infection like bronchitis or pneumonia. Infections can make COPD symptoms much worse, so treating them quickly with antibiotics can help you recover from a flare-up faster. (Some patients with very frequent exacerbations might even take a preventive antibiotic under a doctor’s supervision, but this is specific to certain cases.)
-
Oral corticosteroids: For a severe COPD flare-up (exacerbation), a doctor may prescribe steroid pills like prednisone for a short period (for example, a week or two). These powerful anti-inflammatory medications can help calm a major inflammation in your airways during a bad flare. Because oral steroids can have significant side effects (such as high blood sugar, weight gain, weakened bones, etc.), doctors try to use them for the shortest time necessary and avoid long-term use if possible.
-
-
Oxygen therapy: If COPD has caused your blood oxygen level to be low, you may benefit from supplemental oxygen. Oxygen therapy means you’ll breathe oxygen from a tank or concentrator through a mask or nasal cannula (prongs in your nose). Some people with COPD use oxygen only during exercise or while sleeping, while others with more severe disease may need it for many hours a day or all the time. Using oxygen as prescribed can improve your energy levels, help you stay active longer, and in advanced COPD it can also help you live longer by reducing strain on your heart.
-
Pulmonary rehabilitation: Pulmonary rehab is a special program designed for people with chronic lung diseases like COPD. It usually involves attending sessions a few times a week. In pulmonary rehab, a team of health professionals (such as respiratory therapists, nurses, and physical therapists) teach you exercises to strengthen your breathing muscles and improve endurance. They also provide education on managing your condition, proper breathing techniques (like pursed-lip breathing to help you exhale), nutrition advice, and counseling if needed. Pulmonary rehab has been shown to reduce symptoms and help people with COPD stay active and live more independently.
-
Vaccinations and infection prevention: Respiratory infections can be particularly dangerous for someone with COPD, often triggering severe exacerbations. It’s very important to stay up to date with vaccinations such as the annual flu shot and the pneumococcal vaccine (which helps prevent a common type of pneumonia). If recommended by your doctor, vaccines like COVID-19 should also be kept current. Additionally, practicing good hygiene (like frequent handwashing and avoiding close contact with people who are sick) can help prevent infections.
-
Lifestyle adjustments: Making some changes in daily habits can improve COPD management. Regular light exercise (with your doctor’s approval) can help maintain your fitness and breathing capacity – even walking or gentle cycling can strengthen your muscles. Eating a healthy diet is important; some people with COPD benefit from smaller, more frequent meals to avoid getting too short of breath while eating. Ensuring you get enough rest is also key, as COPD can be tiring. At home, using air purifiers or avoiding exposure to dust and fumes can make breathing easier. If outdoor air quality is poor (for example, on a very smoggy day), it might be best to stay indoors. Also, learn to pace yourself during activities – take breaks and don’t try to rush through tasks that may leave you winded.
For people with very severe COPD that does not improve enough with the treatments above, there are more advanced options:
-
Surgery or specialized procedures: In select cases of severe emphysema (a form of COPD), surgery might be considered. One option is lung volume reduction surgery, where surgeons remove the most damaged portions of the lung. This allows the remaining healthier lung tissue to work better and helps the diaphragm (the main breathing muscle) move more efficiently. There are also less invasive approaches like endobronchial valves, where tiny one-way valves are placed in airways via a bronchoscope (a flexible tube) to collapse diseased parts of the lung and improve breathing in other areas. In the most advanced cases, a lung transplant might be an option – this is when the diseased lung is replaced with a healthy lung from a donor. A transplant can significantly improve breathing, but it is a major surgery with its own risks and the need for lifelong medications to prevent organ rejection. These surgical options are generally reserved for people who have very severe COPD symptoms despite maximum medical treatment and who meet specific criteria.
-
Non-invasive ventilation: Some people with advanced Chronic Obstructive Pulmonary Disease experience a buildup of carbon dioxide or very low oxygen levels, especially during sleep. Doctors may recommend using a machine like a CPAP or BiPAP (bi-level positive airway pressure) at night. This involves wearing a mask over the nose and/or mouth while a machine helps keep the airways open and assists with breathing. This kind of therapy can improve gas exchange (oxygen and carbon dioxide levels) and give the respiratory muscles a rest during sleep, which might help you feel more energetic during the day.
No matter what stage of COPD you have, managing the condition through regular medical care and healthy habits is crucial. COPD is a chronic condition, meaning it requires ongoing attention. By following your treatment plan, taking medications correctly, avoiding smoking, and making the recommended lifestyle changes, you can significantly reduce symptoms and complications. Many people with Chronic Obstructive Pulmonary Disease are able to remain active and enjoy life by managing their condition effectively.
