Osteoporosis is a common bone condition that causes your bones to become weak and more likely to break. It usually develops slowly over many years and often shows no signs until a bone breaks. While it affects both men and women, it’s especially common in women over 50.
In this article, we’ll explain what osteoporosis is, what causes it, the types, common symptoms, how it’s diagnosed, and the treatment options available. We’ll keep things simple, so you don’t need a medical background to understand.
What is Osteoporosis?
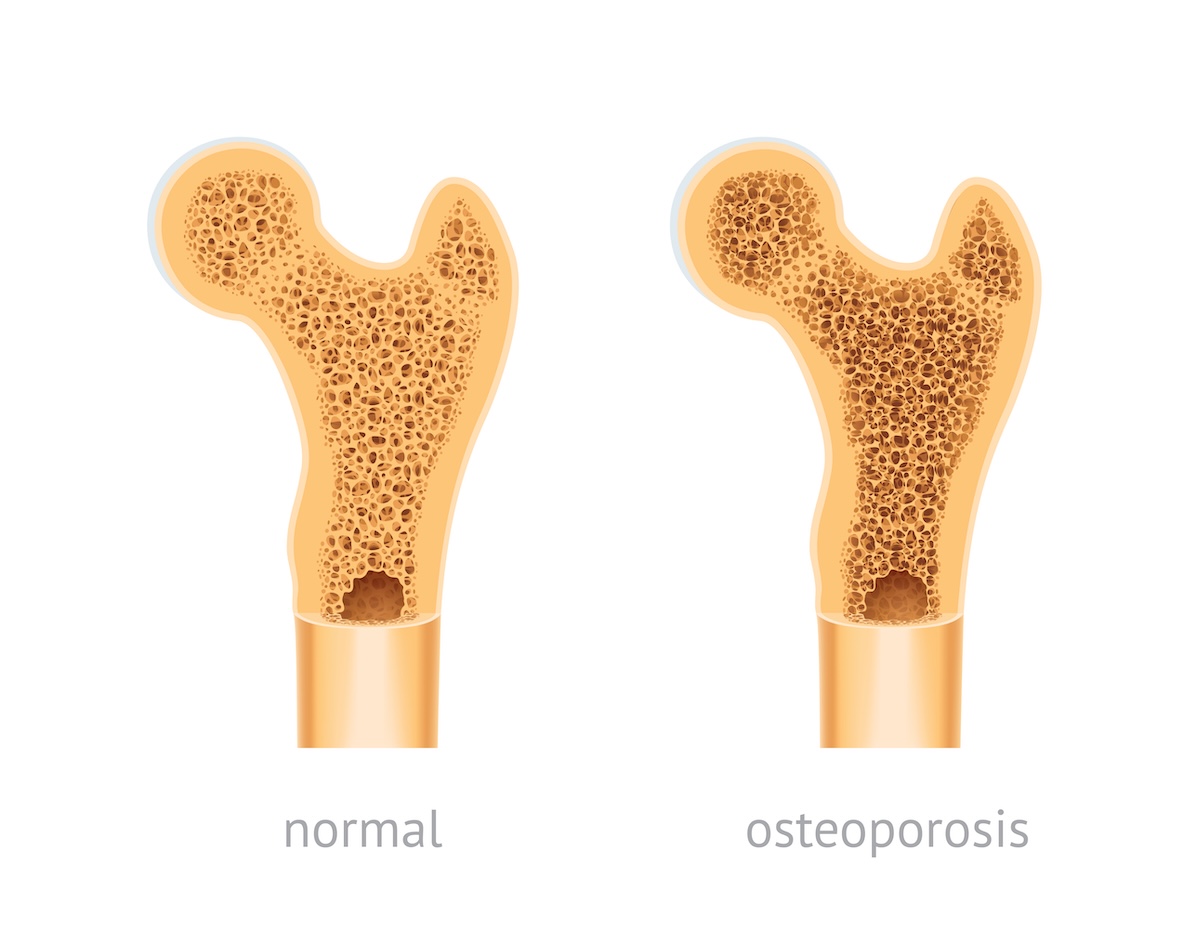
Osteoporosis is a condition where your bones lose their strength and become thinner and weaker. Normally, your body breaks down old bone and replaces it with new bone. But with osteoporosis, this process doesn’t work well. Either too much bone is lost, not enough new bone is made, or both.
When this happens, bones can become so weak that even small movements, like bending over or coughing, can cause a break. The bones that break most often are in the hip, spine, and wrist.
Osteoporosis is a long-term (chronic) condition, but there are ways to manage it and lower the risk of fractures.
What Causes It?
There’s no single cause of osteoporosis, but several things can raise your risk. Age is one of the biggest factors—your bones naturally become less dense as you get older. Women are more likely to get osteoporosis, especially after menopause, when levels of the hormone estrogen drop. Estrogen helps protect bones, and without it, bone loss can speed up.
Other causes include:
-
Low calcium or vitamin D: These nutrients are important for strong bones. Without enough, bones can weaken over time.
-
Lack of exercise: Being active helps keep bones strong, especially weight-bearing exercises like walking or lifting light weights.
-
Smoking and alcohol: Both can harm bone health and increase the risk of bone loss.
-
Certain medications: Long-term use of steroids, like prednisone, can weaken bones.
-
Medical conditions: Diseases like rheumatoid arthritis, celiac disease, and thyroid disorders can also increase your risk.
Family history matters too. If your parent or sibling had osteoporosis or a broken hip, your chances of developing it are higher.
Types of Osteoporosis
There are two main types of osteoporosis:
-
Primary osteoporosis: This is the most common type. It’s mostly caused by aging and hormonal changes, like menopause.
-
Secondary osteoporosis: This happens when another condition or medicine leads to bone loss. For example, long-term steroid use or certain health conditions like kidney disease can cause secondary osteoporosis.
No matter the type, the result is the same—bones that are more likely to break.
Signs and Symptoms
Osteoporosis is often called a “silent disease” because it usually doesn’t cause pain or other symptoms at first. You may not know you have it until you break a bone.
But as the condition gets worse, some people notice:
-
Back pain, especially if a bone in the spine has broken or collapsed
-
Loss of height over time
-
A stooped posture, sometimes called a “hunchback”
-
Bone fractures, especially in the hip, wrist, or spine, from minor bumps or falls
If you notice any of these signs or have risk factors, it’s a good idea to talk to your doctor.
How is Osteoporosis Diagnosed?
Doctors use a test called a bone density scan or DEXA scan to check how strong your bones are. This test is quick, painless, and measures the density of your bones—usually in the hip and spine.
The results give you a number called a T-score:
-
A T-score of -1.0 or higher is normal.
-
Between -1.0 and -2.5 means low bone mass (osteopenia).
-
-2.5 or lower means you have osteoporosis.
Your doctor may also ask about your medical history, lifestyle, and any past fractures. In some cases, blood tests are done to look for causes of bone loss.
Treatment Options
There’s no cure for osteoporosis, but there are many ways to manage it and reduce the risk of broken bones.
Lifestyle changes
-
Eat a bone-healthy diet: Make sure you get enough calcium and vitamin D. Good sources include dairy, leafy greens, fortified foods, and sunlight (for vitamin D).
-
Exercise regularly: Focus on weight-bearing and strength-training exercises like walking, dancing, or lifting light weights.
-
Avoid smoking and limit alcohol: Both can make bone loss worse.
Medications
If your bone density is very low or if you’ve had a fracture, your doctor may recommend medicine. These medicines work in different ways:
-
Bisphosphonates: These are the most common. They slow bone loss and help prevent fractures.
-
Hormone-related therapy: For some women, hormone therapy after menopause can help maintain bone strength.
-
Bone-building medications: For people with very weak bones, drugs like teriparatide or abaloparatide can help the body build new bone.
Your doctor will help choose the right treatment based on your bone density, age, and other health issues.
Living With Osteoporosis
Getting diagnosed with osteoporosis can feel scary, but many people live active, healthy lives with the condition. The key is to take action early and stick with a treatment plan.
If you’ve already had a fracture, physical therapy can help you regain strength and balance. Making your home safer—like using non-slip mats and good lighting—can help prevent future falls.
Stay in touch with your healthcare team, ask questions, and go to regular checkups to monitor your bone health.
