Ischemic heart disease, also called coronary heart disease, is a condition where the blood flow to the heart muscle is reduced or blocked. This happens because the arteries that supply the heart with oxygen-rich blood become narrowed or clogged over time. When the heart doesn’t get enough oxygen, it can lead to chest pain, shortness of breath, or even a heart attack.
This condition is one of the leading causes of death worldwide, but it’s often preventable and manageable with the right care. In this article, we’ll explain what ischemic heart disease is, what causes it, the different types, the symptoms to watch for, how it’s diagnosed, and the treatments that can help manage or even reduce the risk.
What Is Ischemic Heart Disease?
Ischemic heart disease happens when there is a lack of oxygen and blood supply to the heart muscle, usually due to narrowed arteries. These arteries, called coronary arteries, carry oxygen-rich blood to the heart. Over time, fatty deposits called plaque can build up on the walls of these arteries. This condition is known as atherosclerosis.
When plaque builds up, the space inside the artery gets smaller, making it harder for blood to flow. If a piece of plaque breaks off, it can form a clot that blocks the artery completely. This is what causes a heart attack. Even before a heart attack happens, the reduced blood flow can cause other symptoms and weaken the heart over time.
Types of Coronary Heart Disease
There are a few different forms of ischemic heart disease. These include:
-
Stable angina: Chest pain that happens during activity or stress and goes away with rest. It’s a sign that the heart is not getting enough blood when it works harder.
-
Unstable angina: Chest pain that occurs without warning or during rest. It’s more serious and can be a sign of an impending heart attack.
-
Silent ischemia: Reduced blood flow to the heart without any obvious symptoms. Some people, especially those with diabetes, may not feel chest pain even when there is a problem.
-
Heart attack (myocardial infarction): A blockage in a coronary artery that stops blood flow and causes damage to the heart muscle.
All these types are linked to the same underlying issue: reduced blood flow due to narrowed or blocked arteries.
What Causes It?
The main cause of ischemic heart disease is atherosclerosis, which is the buildup of fatty substances and cholesterol on the walls of the arteries. This process can start early in life and progress slowly over time. Several factors increase the risk of developing this condition.
Some of the most common risk factors include smoking, high blood pressure, high cholesterol, diabetes, obesity, a lack of physical activity, and a diet high in saturated fat and sugar. Stress, excessive alcohol use, and a family history of heart disease can also raise the risk.
As these risk factors add up, they damage the inner walls of the arteries, leading to plaque buildup. Eventually, the arteries become stiff and narrowed, and the heart gets less oxygen than it needs, especially during exertion.
Symptoms to Watch For
Symptoms of ischemic heart disease can vary from person to person. Some people experience no symptoms at all until they have a heart attack. Others may have clear warning signs, especially during physical activity or emotional stress. Common symptoms include:
-
Chest pain or discomfort (angina), often described as pressure, squeezing, or fullness in the chest
-
Pain in the shoulders, arms, neck, jaw, or back
-
Shortness of breath, especially during activity
-
Fatigue or weakness
-
Nausea or lightheadedness
-
Sweating without physical activity
These symptoms may come and go. If chest pain becomes more frequent or severe, or if it occurs while resting, it could be a sign of unstable angina or a heart attack and needs urgent medical care.
How It’s Diagnosed
Diagnosing ischemic heart disease usually starts with a physical exam and questions about your symptoms and medical history. If your doctor suspects a problem, several tests may be done to check how well your heart is working and whether your arteries are narrowed.
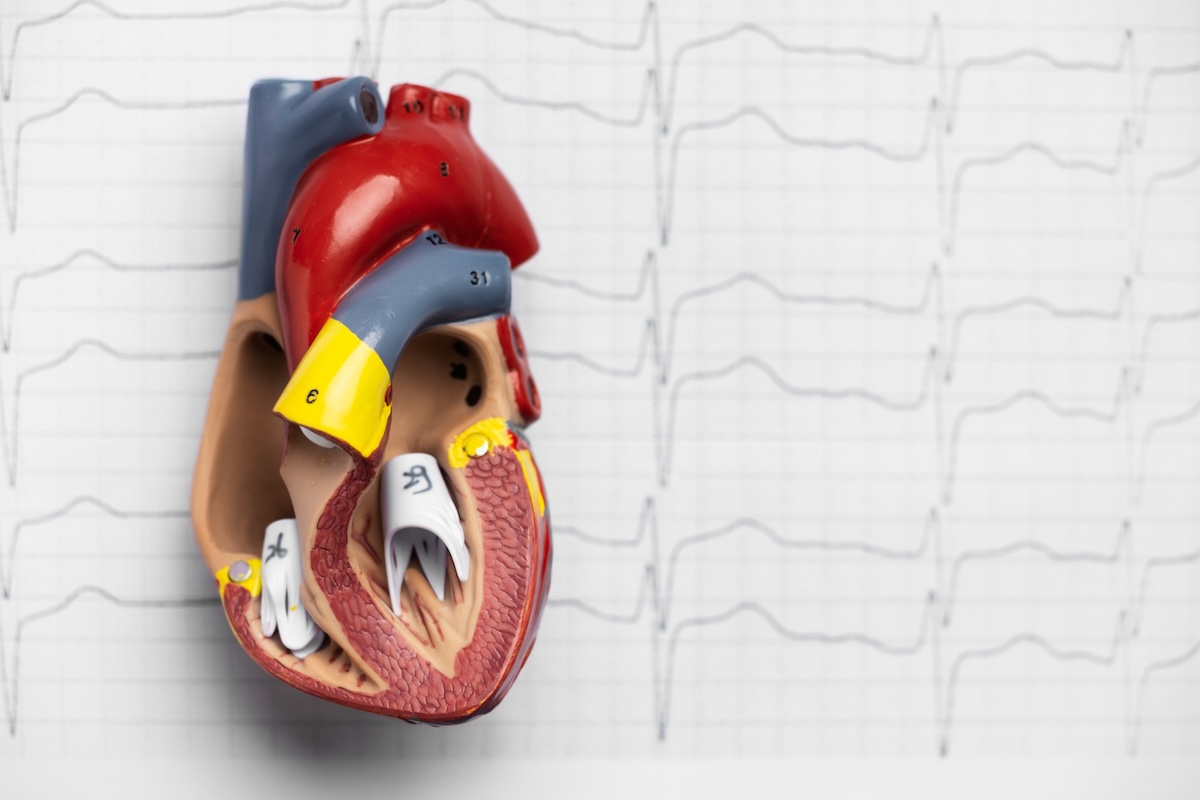
The most common tests include a stress test, which monitors your heart during physical activity, and an electrocardiogram (EKG) to check your heart’s electrical activity. An echocardiogram uses sound waves to create images of the heart and show how it pumps. Blood tests can look for signs of a recent or ongoing heart attack.
Imaging tests such as a coronary angiogram or CT coronary angiography give a closer look at your arteries. These tests help doctors see if there are blockages and how severe they are. Based on these results, your doctor will decide on the best course of treatment.
Treatment Options
The goal of treating ischemic heart disease is to improve blood flow to the heart, reduce symptoms, and prevent serious events like heart attacks. Treatment often starts with lifestyle changes and may include medications or procedures if needed.
Here are common treatment options:
-
Lifestyle changes, such as eating a heart-healthy diet, quitting smoking, getting regular exercise, reducing stress, and maintaining a healthy weight
-
Medications, including drugs to lower blood pressure, reduce cholesterol, prevent blood clots, slow the heart rate, or relieve chest pain
-
Medical procedures, such as angioplasty (using a balloon to open a blocked artery) and stenting (placing a small tube to keep the artery open)
-
Coronary artery bypass surgery, which involves rerouting blood around blocked arteries using a healthy blood vessel from another part of the body
The treatment plan depends on how advanced the condition is and your overall health. Often, a combination of medication and lifestyle changes is enough to control the disease and improve your quality of life.
Living With Ischemic Heart Disease
Being diagnosed with coronary heart disease can be scary, but it doesn’t mean life is over. Many people continue to live full and active lives with the right care and support. Taking medications as directed, attending follow-up appointments, and making healthy choices every day can go a long way in protecting your heart.
Cardiac rehab programs can also help. These supervised programs include exercise training, education, and support to help you recover and reduce future risks.
Managing your condition means staying informed and being consistent. Even small changes—like walking 20 minutes a day or eating more vegetables—can have a big impact over time.
